Understanding Speech and Language Disorders
This film presents an insightful exploration, led by Dr Dinaz Wadia, of the expansive field of speech and language disorders. It serves as a vital resource for anyone seeking to understand the complexities of communication challenges across all ages, from children with developmental delays to adults managing post-stroke aphasia. Through Dr Wadia’s expert insights, the film aims to spread awareness and create a society where people with speech and language disorders are understood and supported.
Actually, when you talk of speech language pathology, it’s a vast field.
It’s…it’s so vast that you can’t just demarcate one area.
And when you’re talking of speech and language, it definitely cannot miss the hearing part because speech and language is going to come in when there is a hearing.
And so audiology is what comes along with speech language pathology, they go hand-in-hand.
Now speech and language, itself, actually, it covers up, basically if you look at it, it’s communication.
So all of this comes into communication disorders, where it affects a person’s quality of life because of an inability to communicate.
And what is communication?
To be able to share, to be able to express, and to be able to receive.
So the baseline of all this comes as receptive and expressive.
So, to, add on to this, let’s look at speech and language disorder as by looking at, at pediatric as well as geriatric.
It’s…it’s a whole gamut of it.
Speech disorder means, he stammers, he is incoherent while speaking, he gets stuck, they can’t think of anything beyond that.
But, let me clarify on that, so when it comes to pediatrics, basically, and when you look at it from the language concepts of it, so if you’re looking at the language, there could be a child, who is not speaking at the age appropriate level, and that’s what you called is delayed.
If by around 18 months if the child is still not speaking, there is a little concern, so that you need to visit a speech language therapist to be able to understand what is the cause.
It could be as simple as environmental causes.
It could be lack of stimulation.
But there could be something more to it which can be missed and if you don’t have the early intervention, you’re missing on the developmental age.
The other aspect is a deviant language development.
It doesn’t follow the norms of development, and so a child maybe speaking a little bit or singing and the parents figure, ‘Oh my child is talking’ but he is not actually conversing, not being able to talk to communicate.
He is using words, off-hand but not using those words meaningfully and intentionally.
As we now recently hear, a lot of kids having the spectrum disorders, so the autism spectrum becomes a part of it.
There could be attention deficit, where the child is not able to learn to speak because of lack of attention.
There could be intellectual deficits, so the cognitive levels are low, and that could be added to it.
There could be speech language disorders which could be associated with disorders like cerebral palsy, it’s a motor neuron neurological problem.
There could be cleft lip and palate, which will have, may have language or not.
Uh, there…there is, more commonly now a days, we’ve seen much more is the apraxia of speech where there is a difficulty of voluntary producing speech, expressing it.
And very, very often which we miss always is, the swallowing disorders.
Children, people think they’re fussy and they’re not eating.
Now there could be many causes, there could be sensory problems or there could be actual swallowing as an issue.
That at times, there’s…there’s a need of other disciplines also to be there.
So we are, we are a team.
The team extends, as I said, from the child, but it can…it be…the medical team, like the pediatrician, the neuro-pediatricians, psychiatrist, psychologist, depending on the need.
The occupational therapist, the physio-therapist, the speech-language therapist, the teachers later on.
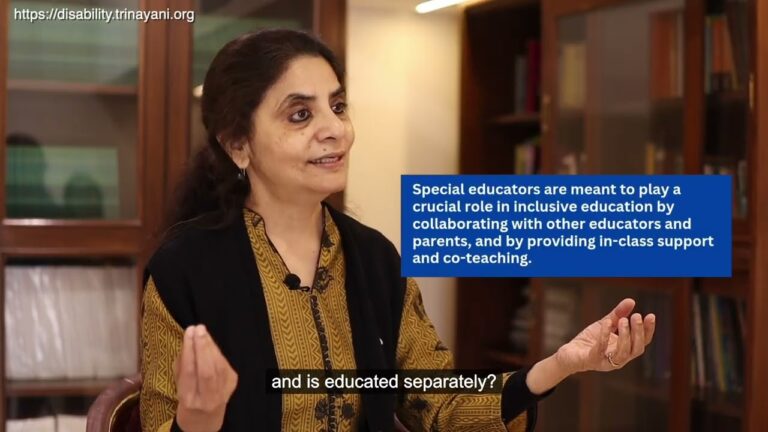
When you talk of inclusion, it’s the school teachers who also come up into it.
Well, language perspectives are lots as far as language is concerned and we have seen it happening more because of the lifestyles.
We’ve seen more of strokes.
The neurological, basically its the neurological problems.
So, post-stroke, post any motor-neuron disorder, there’s a range of it.
But it’s neurological aspects which could cause, things like Parkinson’s, where you have speech language disorders, um the, dementia and Alzheimer’s, they need help in communication.
We have again, what we call as aphasia due to the stroke, where the person may not be able to either understand or express.
And very important, again, here is swallowing.
There’s a whole range of speech disorders which would be in both the groups.
The most commonly occurring which we’ve seen in children would be stammering, not clear, like uh the ‘ka’, the ‘kas’ may be the ‘tas’, the ‘ra’s maybe a ‘la’s, and so it doesn’t sound very intelligible.
And that affects the child’s communication.
What I mentioned is only articulation disorders which is, which also includes when we talk of a lisp, a person is talking with a mild lisp.
Articulation is one part, there’s fluency disorders.
Fluency disorders are where we have a rate of flow of speech, if that flow of speech is interrupted with some hesitations or repetitions, mind you, we all do that, but very little, when it is more, then it is a disorder, which affects communication.
You might find that a person is suddenly talking and quiet, and you’ll feel, ‘doesn’t want to talk’, it may not be that, if a person has the fluency problems.
He might be struggling to get the words.
What we have is disorders of voice.
Voice is the most important thing.
We recognize a person by the type of voice, the quality of voice.
You’re talking on the telephone, you say, ‘oh hi’, even without knowing the name.
And that’s where it’s important.
So, voice deals with three major aspects.
One is the quality, one is incen…intensity, one is the resonance.
These are too technical terms, but intensity means somebody is speaking very softly or somebody is speaking all the time loudly and doesn’t know how to modulate it.
You go to a discotheque or a mall, you’ll naturally raise your voice, but when you’re out of it you’ll naturally lower it.
But a person with a disorder may not be able to do that.
The same way if a person is talking very softly, is not audible, it will affect his communication.
The quality disorders would be where post uh picnic, post too much of talking, you’ll lose your voice.
And so I shouted and screamed, yes, there’s hoarseness of voice but that’s a temporary phase, which may rectify.
But if hoarseness in voice continues, it is a disorder.
It needs to be checked by an ENT specialist, to see the vocal cords, what is the condition and then see what the treatment is needed, medical or therapeutically?
It could be a breathy voice, there could be various disorders depending on how your laryngeal functions are affected.
Uh taking this part of it with voice, I would like to talk a little bit on what is called as Laryngectomy.
Because, that’s the place where, due to CA, or the cancer, or any infection, tumors over there, at times, larynx is removed.
Either it’s partially, completely, it depends on the conditions.
And then, the person’s ability to talk changes.
In the resonance, many people talk a little bit from the nose, the nasal twang, and if it is excessive, it is a disorder because it will affect your sounds, it will affect your clarity.
The other parts…part is what we have is a neurological problem.
But it’s also a speech which goes down with as dysarthria, where there’s a little slurring of speech, where it’s a neurological component, but it has to be attended to.
So, we need to intervene ASAP, as soon as a disorder is identified.
Speech is so important in day-to-day life, in professions and as an adult when a person grows and he’s got to be inclusive and interact, because everything is group discussions nowadays, everything is looked at a group and if I’m not able to communicate, it’s going to hamper.
There could be people misunderstanding you, you might feel conscious of it, you might avoid talking and that interferes with your progress.
Speech and language disorders can be diverse, it covers up a lot of areas and it also manifests in different areas, right from childhood to adulthood, but then most important is quality of life.
For a child, in a school, in a house with friends, for adults, in society, in the workplaces with their colleagues.
So we, as the members of the society, we definitely need to be inclusive.
It’s…it’s such a big thing, inclusion, but are we inclusive?
A person with a challenge immediately catches attention to the public.
You’ll immediately look or you’ll smile or maybe you’ll…you’ll make an expression and that individual is so sensitive, it’s going to affect.
If it’s a child, a response from the other students, if it’s a person in the office, his colleagues.
So, let us be more aware and more empathetic.
I do not want you to be sympathetic, nobody wants, nobody wants pity, but they want to be understood and if you can’t understand, maybe ask them.
They’ll be able to explain the challenges.
But we need to cover up this area, of giving them enough time to speak, giving them the opportunity to express, with whatever challenges they have, and that’s the best thing which you can do.
Some of the teaching materials which we can use, therapy materials I would say, are different types of toys and aids which can help them in learning speech and language.
Toys, picture cards, flash cards, books, the therapy aids and the materials depend on the needs of the child and it has to be planned with, with the targets which you have.
So sometimes you have very big pictures, sometimes you have smaller pictures and sometimes there’s still smaller flash cards.
So, depending on what the child wants, depending on the level of functioning and the strengths of the child, you choose materials ranging from flashcards, books, pictures, uh toys, teaching aids, puzzles: one, one piece puzzles to ranging to multiple piece puzzles.
My suggestion to the parents is just, just don’t go to the market and pick up all this because they have to be adequately selected, keeping in mind the needs of the child and with advice by a professional.
This is, as I mentioned, the hearing and speech and language go hand-in-hand, the hearing assessments can be done in an audiometry set-up.
This is a very small set-up, where you have an audiometer and it’s a sound treated room where the assessment can be done but in a hospital set-up or in other private set-ups you can have more done.
Uh hearing assessment for children, fortunately nowadays has become more or less mandatory at birth, and especially for children with high risk, they need to be assessed so that the development is taken care of and the parents need to be in regular touch with the medical professional to regularly update the assessments.
Very important to understand the therapy is individualized, depending on the needs of each individual, a child or an adult. So, it’s always good to…assessment to understand and then do the therapy.
articulation disorders, audiology, autism spectrum, Cerebral Palsy, communication disorders, fluency disorders, geriatric speech therapy, hearing assessment, inclusivity, language development, laryngectomy, neurological disorders, pediatric speech therapy, quality of life, speech disorders, speech language pathology, speech therapy materials, stroke rehabilitation, swallowing disorders, voice disorders
Dive Deeper: More on Disability
Learn about the most common inquiries surrounding disability, education, legislation, accessibility, employment and other sectors related to disability.


Playlist
Access & Inclusion


Playlist
Adaptive Sports


Playlist
Alternative Communication Methods


Playlist
Autism & Neurodiversity


Playlist
Blindness & Adaptations


Playlist